Public and Patient Involvement in FReSH START
We believe public and patient involvement (PPI) in mental health research is vital: the best way to improve services is to make sure we are listening to the voices of the people who need them.
What does this look like in practice?
In FReSH START, we built PPI into the whole process. The programme aims were developed by academics and members of the public with personal experience of self-harm, and it was this collaboration that helped revise the study design. One example was the decision to make the primary outcome quality of life rather than reduction in self-harm because people with experience were clear that this is more relevant to them.
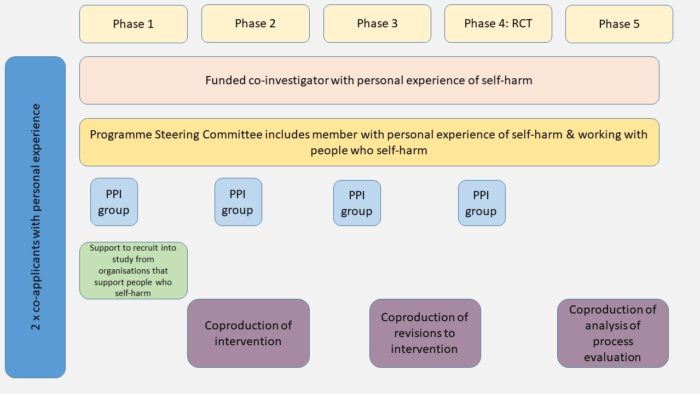
Patients and the public have been involved in the programme in 6 different ways: as co-applicants, on the Independent Steering Committee, as coinvestigators on the Programme Management Group, through HEER (Help from Experts by Experience in Research at Leeds and York Partnership Foundation Trust), in the service user reference group, and at a series of coproduction workshops.
All these different levels of involvement ensure we are truly involving, and not just consulting.
Manchester co-production workshops – PPI in action
One part of our work that has been key to the development of the intervention so far, is the coproduction workshops we held in Manchester in autumn 2019. The workshops brought together the research team, 11 people with experience of self-harm, and 6 expert therapists, to modify three therapies to support people who self-harm.
There were practical things we felt were important to make sure everyone in the group was involved as equals. Rather than being managed by the research team, the workshops were co-designed and led by a skilled facilitator who herself had experience of self-harm. We chose to hold each day in a different community-owned venue. This meant that we were all visitors but also that we were able to financially support local organisations. All participants were paid for their time and expertise, as well as being reimbursed for travel expenses, with lunch provided by a local independent caterer.
Here is an outline of how we structured these workshops:
Workshop 1: People with experience of self-harm worked with researchers to interpret findings from a review of the strategies people have found helpful in reducing or managing their self-harm. This workshop helped us to understand how these strategies could be incorporated into the therapy sessions and what language should be used when discussing them.
Workshop 2: The same group of people discussed findings from our study that explored people’s reasons for self-harm. This helped us to identify how these findings could be used in therapy and what might not work well for patients.
Workshop 3: We took all the information from the first two workshops and the expert therapists discussed how these could be used to modify the three therapies. One PPI consultant also took part to help us to clarify questions or identify further concerns.
Workshop 4: All the therapists, 4 members of the research team, and 11 people with experience of self-harm came together to explore the modifications made to the therapies, and further understand how and why the therapies might or might not work for patients.
How did it go?
It was, at times, a moving and challenging process for everyone involved but we had great feedback from the group. In particular, participants with experience of self-harm were excited to be part of creating something positive for people in the future even if they wouldn’t benefit from the therapies themselves. Therapist participants found it helpful to hear how patients might respond to hearing other people’s reasons for self-harm and ways of managing it. They returned to workshop 4 with a new proposal for approaching the question of self-harm during therapy and the group were able to adapt the kind of language to be used during therapy sessions.
What questions did it raise for the rest of the programme?
The process was far from smooth and we felt there were still many more questions to think about:
How can we better support our team and PPI contacts? Key to the success was our advisor and facilitator who herself has experience of self-harm, but it was a tough mediating role for her to take on.
How can we feedback regularly and maintain the relationship without over loading participants?
How do we increase the diversity of representation in the group?
Do we really place equal value on all forms of knowledge?
How can we do it better next time?
What are our future aims?
PPI is always a work in progress so we are flexible in what we do. We are open to adapt what we do and how we do it according to the input we get from our PPI advisors. Some of the things we will be focusing on over the next three years are:
Creating a patient and public reference group: 8-15 people who will work with us to ensure that what we do is PPI-led. This might include helping to analyse qualitative data, and revising patient facing materials, but we are keen that the group tell us how they would like to be involved.
Diversity: We acknowledge that people from ethnically diverse communities have been widely underrepresented within academic research, and we have a responsibility as researchers to change this for the future. We are working closely with peer-led organisations supporting people from diverse groups to gradually build their trust, in us and our research, and encourage meaningful involvement through our PPI work.
Mentoring individuals: We will be pairing up our researchers with people with experience of self-harm a) to support their involvement in research, and b) to work with us to engage with and involve people who have difficulty taking part in research. This will include young people in communities where there is particular stigma associated with self-harm.
Continue to pay members of the group for their expertise and time: we believe that a) it is important to acknowledge the time and expertise all members provide and b) one of the barriers to power sharing is that the professional members of the team (like researchers and clinicians) have salaries whilst the PPI members may not be paid at all.
Be adaptable and use different ways of working: we hope to be able to hold some face to face groups, but also make sure that video groups are manageable for everybody by keeping them short to avoid ‘Zoom fatigue’, and inviting participation by email or telephone if people prefer this. We will be asking for brief anonymous feedback after each significant engagement so that we can learn and improve how we work as we go along.
